Each year, millions of births still occur without any assistance from a skilled attendant despite recent progress
Ensuring that all births are assisted by skilled health personnel is critical for reducing maternal and newborn deaths. Skilled health professionals assisted 86 per cent of births globally in 2022, but coverage continues to be uneven around the world with significant discrepancies between regions. While regions like Europe and Central Asia, North America, Latin America and the Caribbean, and the Middle East and North Africa have achieved universal or nearly universal coverage, only 70 per cent of births are attended by a medical doctor, nurse or midwife in sub-Saharan Africa. According to projections, sub-Saharan Africa will experience a 15 per cent increase in the number of annual births between 2020 and 2050. If current coverage of births by skilled health personnel stays the same, approximately 141 million births in sub-Saharan Africa will occur without the assistance of skilled health personnel between 2022 and 2030. Taking into account the projected population changes in regions like sub-Saharan Africa, substantially more resources will be required to increase intervention coverage levels and provide skilled care to women and their newborns during childbirth.
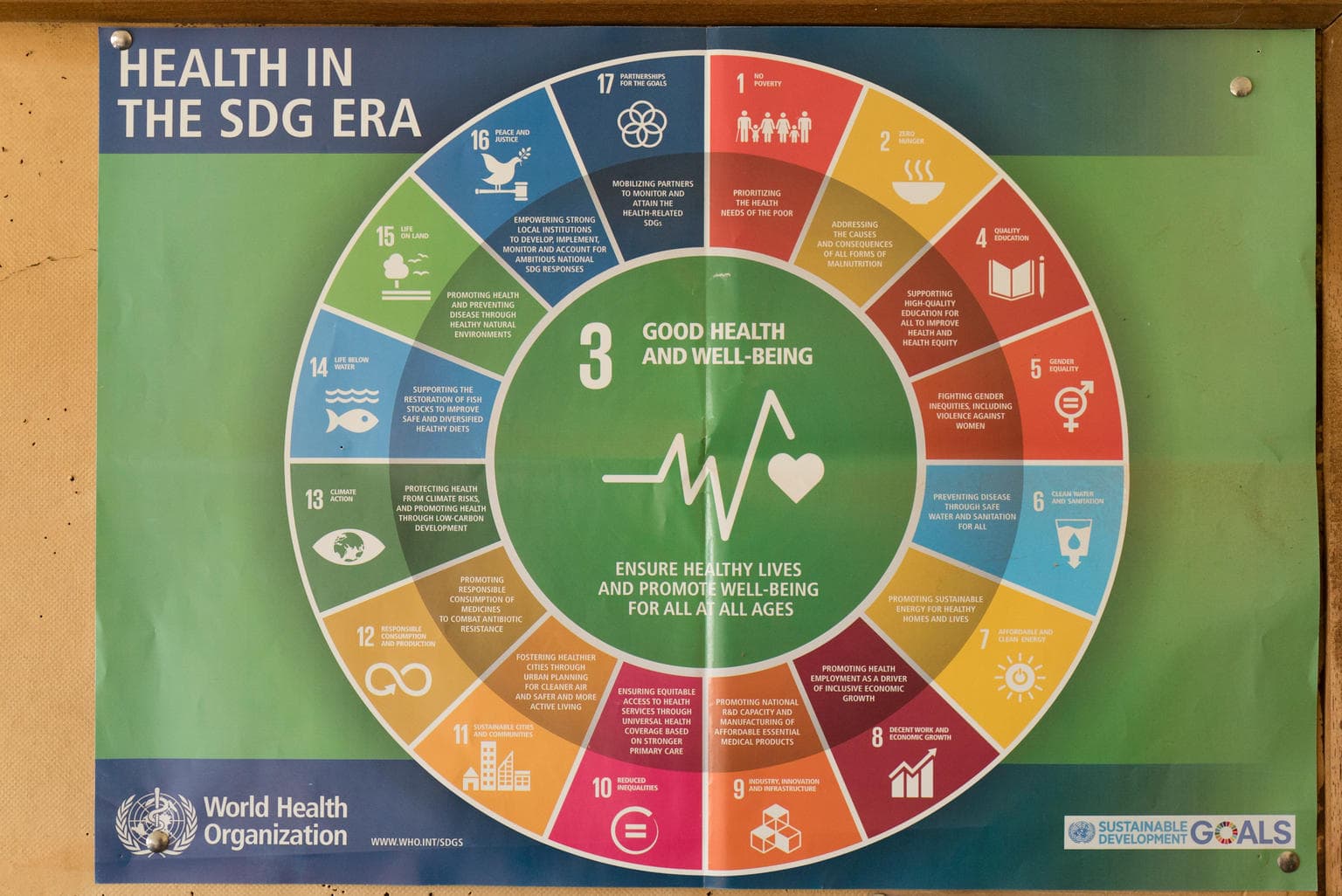
Skilled health personnel, including medical doctors, nurses and midwives, are trained to handle normal deliveries safely. They are also able to recognize warning signs for complications and refer mothers to emergency care in case of complications like haemorrhage or sepsis, which are the leading causes of death among mothers during and after childbirth. Reflecting its importance in reducing maternal morbidity and mortality, the proportion of births attended by skilled health personnel was included as indicator 3.1.2 under Goal 3 and Target 3.1 of the Sustainable Development Goals.
Despite facing challenges in increasing skilled care at birth, sub-Saharan Africa and Southern Asia are the regions with the greatest progress globally in increasing coverage of births assisted by health professionals. Since 2000, coverage of births by skilled birth attendants in the sub-Saharan African regions has grown by approximately 35 percentage points while South Asia has grown by over 50 percentage points.
Adolescent mothers
Currently, the highest rates of early childbearing are found in sub-Saharan African countries, where birth rates among adolescents in 2022 reached 99 births per 1,000 girls aged 15-19, compared to lower rates in other regions. It is important that girls in this vulnerable group receive an education on family planning as well as the necessary care during pregnancy and childbirth to ensure their wellbeing and the wellbeing of their babies.
Disparities in coverage
Despite progress made in the past decade, large equity gaps remain, with rural and poor populations often left behind. Globally, in 2022, approximately 76 per cent of births among rural mothers were attended by skilled health personnel, compared to 93 per cent of births among urban mothers.
Large disparities in care during childbirth are also observed across wealth quintiles. Globally in 2022, women in the richest 20 per cent of the population for their country were around 1.5 times more likely than women in the poorest quintile to have a skilled birth attendant at delivery (96 per cent versus 67 per cent). Differences across wealth quintiles are largest in West and Central Africa with the richest being 2 times more likely to deliver with the help of a skilled health provider than the poorest (94 per cent versus 45 per cent).
Institutional deliveries
Monitoring deliveries in health facilities is essential to ensuring that women receive quality care and deliver in an environment that is prepared for an emergency. In many countries, particularly middle- and high-income countries, a large proportion of babies are delivered in health facilities. Giving birth in a health facility can increase survival prospects for mother and baby through access to appropriate equipment and supplies that are available on site or through immediate referral to a higher-level facility. However, it remains essential to also ensure that the delivery is carried out by skilled health personnel who are capable of anticipating or detecting signs and symptoms of complications. In addition, it is critical that water, sanitation and hygiene services are available in health care facilities. This is key for infection prevention and control, patient safety and child and maternal health, particularly during the time around child delivery.
Over 9 in 10 births occurred in health facilities in Eastern Europe and Central Asia (98 per cent), East Asia and the Pacific (89 per cent) and Latin America and the Caribbean (94 per cent). In contrast, in West and Central Africa and Eastern and Southern Africa, where the burden of maternal and newborn deaths is highest, 63 and 62 per cent of births respectively were delivered in health facilities. In sub-Saharan Africa, there was an urban-rural gap of 27 percentage points (81 per cent vs 54 per cent) and a staggering 47 percentage point gap between women in the richest (90 per cent) wealth quintiles and those in the poorest (43 per cent) wealth quintiles.
Caesarean section
A caesarean section, or C-section, can be a life-saving intervention and is an essential part of comprehensive emergency obstetric care, preventing maternal and perinatal mortality and morbidity when medically justified. Globally in 2022, approximately 18 per cent of newborns were delivered by C- section. In Latin America and the Caribbean, C-sections accounted for 46 per cent of all deliveries, almost 10 times higher than in sub-Saharan Africa (5 per cent). Latin America and the Caribbean’s high coverage of C-sections may suggest over-medicalization of childbirth; conversely, the low percentage of C-sections in sub-Saharan Africa (5 per cent) is alarming, suggesting a dire lack of access to this potentially lifesaving intervention.
Globally, the proportion of babies delivered by C-section in urban areas is twice that of those in rural areas (21 per cent and 11 per cent, respectively), although the disparities are relatively small in sub-Saharan Africa (8 per cent and 3 per cent, respectively) where overall C-section deliveries are the lowest.
References
United Nations Inter-agency Group for Child Mortality Estimation (IGME), Levels and Trends in Child Mortality, UNICEF , New York, 2023.
WHO/UNICEF JMP, Progress on household drinking water, sanitation and hygiene 2000-2022: Special focus on gender, UNICEF, New York, 2019., UNICEF, New York, 2023.
UNICEF, State of the World’s Children 2023, UNICEF, New York, 2023.
UNICEF, Healthy Mothers, Healthy Newborns: Taking Stock of Maternal Health. UNICEF, New York, 2019.
UNICEF, Committing to Child Survival: A Promise Renewed – 2015, UNICEF, New York, 2015.
WHO, UNFPA, UNICEF, AMDD, Monitoring Emergency Obstetric Care – A handbook, 2009 revision, WHO, Geneva 2009.
WHO, UNICEF, UNFPA and The World Bank, Trends in Maternal Mortality: 2000 to 2020, WHO, Geneva, 2023.
UNICEF, Delivering for women: Improving maternal health services to save lives, UNICEF, New York, 2022.
Delivery care
Maternal and Newborn Health Coverage
Build and download your own customisable dataset
Resources





Notes on the data
UNICEF – in collaboration with WHO – is the custodian agency responsible for monitoring and reporting “Proportion of births attended by skilled health personnel”, an official indicator for Goal 3 of the Sustainable Development Goals.
| Sustainable Development Goal | Target | Indicator |
| Goal 3: Ensure healthy lives and promote well-being for all at all ages |
Target 3.1: By 2030, reduce the global maternal mortality ratio to less than 70 per 100,000 live births |
3.1.2: Proportion of births attended by skilled health personnel (doctor, nurse, midwife) |
Definition:
The proportion of births attended by skilled health personnel as defined as the percentage of live births attended by skilled health personnel (doctor, nurse, midwife).
Computation:
The indicator is computed as the number of live births attended by skilled health personnel out of total number of live births in a specified reference period.
Limitations:
Standardization of the definition of skilled health personnel can be challenging on account of differences in training of health personnel across countries. Although efforts have been made to standardize the definitions of doctors, nurses, midwives (and in some cases, auxiliary midwives) used in most household surveys, it is likely that the abilities of many skilled attendants to provide appropriate care in an emergency depends on the environment in which they work. Additionally, this indicator is a measure of a health system’s ability to provide adequate care for pregnant women; however, concerns have been expressed that the presence of a skilled attendant may not adequately capture women’s access to good-quality care, particularly when complications arise, and that information on the supplies and equipment a skilled attendant may or may not have is lacking.
Database:
Since 2015, UNICEF and WHO have maintained a joint database on skilled attendant at birth. Joint estimates are published annually, released simultaneously in May by UNICEF and WHO in the State of the World’s Children report, and are available at www.data.unicef.org and World Health Statistics (http://www.who.int/whosis/whostat/en/), respectively. As skilled attendance at delivery is an SDG indicator (3.1.2), databases and regional estimates are also provided for SDG data releases on an annual basis.
